What are the risks of coronavirus COVID-19 for people living with hepatitis B or hepatitis C? People with weakened immune systems (e.g. people on immune suppressing medications, people receiving cancer treatments), older people especially those aged over 70 years, Aboriginal and Torres Strait Islander people and people with chronic medical conditions are particularly at risk from the effects of COVID-19.
This means some people living with hepatitis B and hepatitis C could be at greater risk of serious health complications if they become infected with COVID-19. In particular, if you have had hepatitis B or hepatitis C for some time, and have developed advanced liver diseases (including cirrhosis), this makes severe COVID-19 illness more likely. This includes people who have ongoing health conditions as a result of a previous hepatitis C infection, even if that infection has been cured.
If you have hepatitis B or hepatitis C, or have previously had hepatitis C, the COVID-19 crisis is a good reminder to consider asking your doctor for a liver health check if you have not had one in the last six months. Be vigilant, use basic measures to protect yourself against COVID-19, and consult a healthcare provider if in doubt about your risk, especially if you have been around someone who has travelled overseas recently.
People with significant liver disease are recommended to receive vaccinations against influenza and pneumococcal disease. These are funded for people aged 65 and over, and influenza vaccine is funded for all people with chronic liver disease. It is a good idea to make an appointment with your GP to discuss vaccination as soon as possible.
It is important that people with gastrointestinal and liver conditions remain under care through the COVID-19 outbreak.
If you are currently taking treatment for hepatitis B or hepatitis C, or other chronic conditions, it is recommended to ensure you have an adequate stock of your medication to reduce unnecessary visits to health services or pharmacies. Your medications were prescribed to manage your medical condition and to keep your condition well controlled. Stopping medication poses a risk of poor disease control. Any adjustments to your medications should only occur in discussion with your treating clinician. If you are unwell with COVID-19 then the doctors treating you may temporarily stop some of your medications. Your specialist should be notified if this happens as alternative medications may be required.
It is important that people with gastrointestinal and liver conditions remain under care through the COVID-19 outbreak. Hospital clinics and specialists are reducing the numbers of people attending for routine review. Some people with active issues of concern may need to be seen for a face-to-face consultation.
However, from 13 March 2020 tele-consultations with a specialist via video-conference is covered by Medicare. As older people and those with chronic illnesses or who are immuno-suppressed may be at increased risk if they develop COVID-19 infection, these video-conference consultations provide a way of receiving specialist review of your condition without the infection risk associated with visiting the clinic. Contact your specialist to discuss whether a tele-health consultation is appropriate for you.
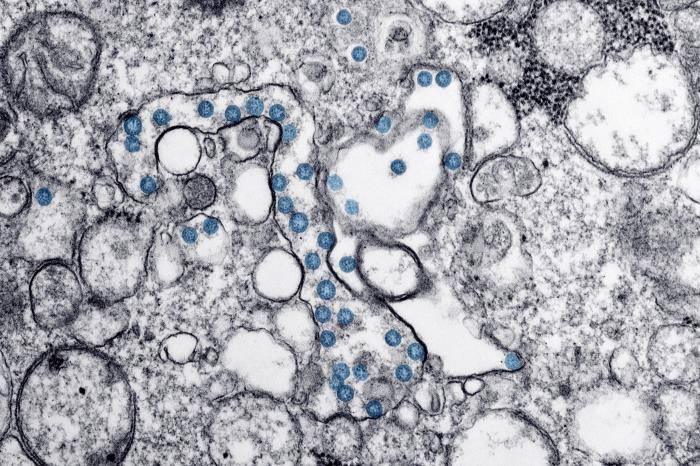
About COVID-19
COVID-19 is a coronavirus. Coronaviruses can make humans and animals sick. Some coronaviruses can cause illness similar to the common cold and others can cause more serious diseases, including Severe Acute Respiratory Syndrome (SARS) and Middle East respiratory syndrome (MERS). This new coronavirus originated in 2019, and so this disease outbreak is named COVID-19.
The coronavirus is most likely to spread from person-to-person through:
- direct close contact with a person while they are infectious
- close contact with a person with a confirmed infection who coughs or sneezes, or
- touching objects or surfaces (such as door handles or tables) contaminated from a cough or sneeze from a person with a confirmed infection, and then touching your mouth or face.
The virus causing COVID-19 infection has not previously affected humans. This means there is no immunity to this infection in the community. Practising good hand and sneeze/cough hygiene is the best defence against most viruses. Face masks are not routinely recommended for members of the public, unless they are already sick.
You should:
- wash your hands frequently with soap and water, before and after eating, and after going to the toilet
- cover your cough and sneeze, dispose of tissues, and use alcohol-based hand sanitiser
- and if unwell, avoid contact with others (stay more than 1.5 metres from people).
The virus will affect individuals differently. Many people who come in contact with the virus will experience a mild illness or no symptoms at all, but some can go on to develop serious effects such as pneumonia. People with COVID-19 most commonly experience:
- fever
- flu-like symptoms, including coughing, sore throat and fatigue
- shortness of breath
If you have a fever, cough or other symptoms, seek medical care early. If you think you could have contracted COVID-19, you should call ahead before visiting a doctor. If you have serious symptoms, such as difficulty breathing, call 000 for urgent medical help.
The influenza vaccine provides optimal protection for the first three to four months after vaccination. People within one year of liver transplantation are recommended to have a second flu-shot at least four weeks after the initial vaccination. Pneumococcal vaccination every five to ten years is also recommended for people with reduced immunity. Specific recommendations vary according to age and previous vaccination history.
If you are a smoker, cigarette smoking also increases the risk of severe respiratory illness, and quitting smoking may reduce your chances of complications due to COVID-19.
Remember, taking action sooner rather than later is advised, as increasing numbers of people in the general population infected with COVID-19 will put more strain on the healthcare system, making it harder to get appointments or visit medical clinics or hospitals.
Where can you get more information about COVID-19?
You can get additional information about COVID-19 on the Department of Health website:
https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert
You can also contact the Coronavirus Health Information Line on 1800-020-080. This line operates 24 hours a day, 7 days a week.
In South Australia, contact the South Australian Department of Health on 1300 232 272, or visit https://www.sahealth.sa.gov.au/
For information in languages other than English visit: http://bit.ly/covid-lote
Advice in this article was drawn from:
– Coronavirus disease (COVID-19) What you need to know – from the Australian Government Department of Health
– Coronavirus COVID-19 factsheet for people affected by hepatitis B and hepatitis C – from Hepatitis Australia.
– Impact of COVID-19 on patients with gastrointestinal or liver disorders – from the Gastroenterological Society of Australia.